Ankle Sprain
Ankle Sprain
Most people will experience an ankle sprain at some point in their life, ankle sprains are the most frequently seen sports injury and are particularly prevalent amongst professional athletes.
The most common cause is the internal rotation of the foot. Sprained ankles can also be caused by eversion (an external rotation of the foot) and sometimes both injuries can coincide. The ligament most prone to an inversion injury is the anterior talofibular (ATFL) followed by the calcaneal fibular (CFL) and the posterior talofibular (PTFL). While eversion injuries more often result from an injury to the deltoid ligament,. The swelling is usually immediate and pain can be very intense,. Movement is severely limited due to the swelling, whilst the ankle’s stability can also be affected in more severe cases.
If the area around the ankle is remarkably swollen, an X-ray is usually performed to rule-out the presence of any fractures. An ultrasound performed a few days after the injury can help to highlift distortion or ligament damage. In rare cases, the examination can be complete with an MRI or CT scan.
Rehabilitation following acute traumatic injuries is crucial for the restoration of joint stability and for it to function dynamically. It is also important that the patient continues a maintenance program once their rehabilitation is complete in order to avoid the problem recurring.

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.
Osteoarthritis of the Knee
Osteoarthritis of the Knee
Osteoarthritis is a very common condition, which is mainly degenerative and characterized by wear and aging. In rare cases, it may occur at an early age, originating from a traumatic injury if not properly treated. This degenerative phenomenon often resists attempts to reduce pain, instead formation of periarticular ossifications (osteophytes) can cause disabling restrictions to movement. This condition can occur in otherwise healthy joints affected by altered joint mechanics, or due to malformations caused by previous injuries. It is particularly prevalent in women and overweight patients. In those suffering from this condition, repetition of certain movements or flawed posture can cause irreversible damage to joints in the long run.
Symptoms are well defined in these cases; pain, swelling, limp walking, feelings of resistance in the joints and cracking noises from joints during activities all point towards this diagnosis.
To reach a definitive diagnosis, clinical and radiological methods are typically used. X-rays provide a good picture of any abnormalities in the skeletal profile, whilst CT and MRI scans can detect abnormalities in cartilaginous tissues.
Well-designed rehabilitation programs can improve the quality of life for those suffering, by reducing pain and restoring range of motion to the joint therefore slowing an advancement of the condition. As always, we believe that improving movements through therapy is fundamental to success. There are some basic guidelines patients should follow to reduce the effects of osteoarthritis. These include weight loss, or conversely avoiding excessive physical exercise, as well as maintaining correct posture during both day and night.

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.
Iliotibial Band Syndrome
Iliotibial Band 'ITB' Syndrome
This term indicated a framework of chronic inflammation that affects the last section of the fascia lata (iliotibial section) where there may be mechanical friction that generates a painful inflammation condition, felt most during movements of flexion and extension of the knee. This syndrome is particularly prevalent among footballers, runners, and cyclists and it may arise from overloading of the joints, or from training on hard or irregular surfaces. Some anatomical factors may increase the incidence of the disease, such as varus knee and hypo-extensibility of the posterior muscular chain. The main symptom is pain at the lateral part of the knee. Sometimes there is also swelling at the insertion points of the tendons. Sport is often made impossible due to pain and the feelings of stiffness that accompany it.
The diagnosis is essentially clinical. Ultrasound can help in confirming the diagnosis and showing the degree of inflammation. Magnetic resonance imaging (MRI) may be useful in the differential diagnosis between this and an external meniscal condition. The treatment is almost always conservative and consists of a mix of physical and manual therapy. In the acute phase it is necessary to reduce, change, or suspend sporting activity depending on the severity of the situation. Surgical solutions can be considered in selected cases where resistance to the conservative treatment is found.

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.
Patello-Femoral Syndrome
Patello-Femoral Syndrome
This consists of a group of moropho-functional alterations that results in the onset of anterior knee pain.
The patella moves inside a cavity, dug into the distal part of the femur; bone surfaces slide over one another, facilitated by cartilage covering them and are guided by the tension of certain muscle groups like the patellar tendon and alar ligaments. A small alteration of form or function in ofe of these components is enough to increase the pressure on one part of the patellofemoral joint with consequent onset of pain or, even worse, instability which can lead to the patella leaving its seat in painful episodes of dislocation. Diagnosis relies on support from X-rays and CT or MRI scans. Rehabilitation begins in the gym, but continues through everyday like when patients will need to put small changes into place to maintain full functionality. The only real cause for surgical treatments is the presence of major patellar instability, characterized by habitual dislocation of the patella or its on-going mapostion. Surgical interventions include the realignment of the extensor apparatus, which can be performed arthroscopically or with open surgery. There are many ways to deal with this as the origin of instability is often due to many different factors. Howcer, this decision is always taken by an orthopedic surgeon specialised in knee surgery, who will always account for all the different factors affecting the patient. After, surgery rehabilitation aims to restore full function in the knee, first resolving the inflammation, then recovering the range of motion, followed by muscle strength, and finally the more sophisticated movements used in everyday life or the patient’s chosen sport.

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.
Patellar Tendiopathy
Jumper’s Knee ‘Patellar Tendiopathy’
This is a very common disease affecting athletes who use explosive strength (in volleyball, basketball, and athletics for example). This can be the result of an acute event due to a functional overload, or the result of repetitive microtraumas. Clinically, pain is noted at the inferior pole of the patella accompanied by painful swelling. The pain builds gradually, decreases after warming up but then gradually intensifies, limiting performance.
There are 4 clear clinical stages to this condition:
Stage I: pain appears after training, activity is not limited
Stage II: pain is initially present, disappears after warming, then reappears again after that
Stage III: the pain persists for the whole duration of the play/ movement
Stage IV: tendon rupture
The diagnosis is usually only clinical, supported by ultrasound scans of the muscle-tendon to get an idea of the degree of tendinosis, or an MRI for the most severe cases. For all but the most severe cases (complete tendon rupture), conservative treatments are more commonly used. The course of treatment here is quite a delicate process, where success is based upon the severity of injury and the time taken to start after the onset of symptoms.

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.
Meniscus Tear
Meniscus Tear
A lesion of the meniscus may occur during the combined movements of flexion and rotation typical in traumatic distortions. A lesion may also occur, however, after a banal movement or through cartilage degeneration and loss of elasticity in elderly people. Symptoms vary from an acute sting localized along the articular line to a dull and undefined pain that flares up during certain movements. Important meniscal lesions may generate a real articular block which most of the time can be resolved with appropriate titling maneuvers in flexion-extension.
During the examination different parameters will be evaluated such as finding the exact area of pain, swelling, defining the range of motion and the presence of any looseness. The tests used to confirm the diagnosis include magnetic resonance imaging (MRI) or computer tomography (CT) due to their ability to show both skeletal components and muscular structures. An accurate diagnosis is crucial in order to plan a suitable rehabilitation program. This will be differentiated based on the type of lesion and the patient’s unique needs. Conservative (non operative) methods are effective for many cases but based on the severity of the injury, surgical intervention may be necessary.

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.
Carpal Tunnel Syndrome
Carpal Tunnel Syndrome
This syndrome forms as the result of compression of the median nerve as it passes through the carpal tunnel (wrist tunnel), formed by the carpal bones and the flexor tendons of the fingers and wrist. The most common causes of this are thickening and swelling of the tendon sheaths or the irregularity or enlargement of the carpal bones due to osteoarthritis. Alternatively, chronic conditions such as amyloidosis, diabetes mellitus and rheumatoid arthritis as well as hormonal changes due to pregnancy or menopause can narrow the diameter of the carpal tunnel, compressing the median nerve. Finally, fractures to the wrist can also cause damage to the median nerve, bringing on the onset of this condition. Initial symptoms include nocturnal disturbances as a result of tingling/ numb sensations in the hand and fingers. Patients frequently discuss difficulties in performing delicate tasks like tying shoelaces or buttoning up thier shirts. After some time, these feelings of tingling evolve into feelings of pain, especially during movement, that persists throughout the day. Given the fact that motor fibers are also often involved in this condition, the nerve supply to the thumb muscles can be affected, leading to weakness and wasting. Diagnosis of this disorder is based on specific clinical tests backed by electromyography (EMG) test to confirm the extent of nerve degeneration. Depending on the patient’s clinical history, other tests such as blood tests, X-rays and CT scans may be useful in cases of secondary forms of this disorder. Prognosis here generally leads to a total absence of any sensory disturbances after a few months. Rehabilitation using splints and physical treatments to address the muscular imbalances, especially those in the wrist and forearm, is key for the restoration of fine motor control. In more advanced cases where motor components are affected, a surgical procedure known as ‘carpal tunnel release’ may be required to prevent irreversible damage to the nerve and the muscle it supplies.

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.
Epicondylitis
Tennis Elbow / Golfer’s Elbow ‘Epicondylitis’
This painful syndrome is localized around the lateral (outside) epicondyle (the bony protrusion of the humerus) and can be called ‘tennis elbow’, lateral epicondylitis, or epicondylalgia. In the majority of cases, this presents itself due to a series of microtraumas to the tendon in the wrist and the hand’s extensor muscles near to where the tendon attaches to the epicondyle. Conversely, ‘golfers’ elbow’ (or medial epicondylitis / epicondylagia) is characterized by pain on medial (inside) epicondyle, caused by microtraumas to the flexor tendons of the hand and wrist. Repetitive movements in the presence of muscular imbalances result in changes occuring in the tendon of either (or both) the medial or lateral medial epicondyle.
Problems are more prevalent in certain sports such as golf or tennis, or certain occupations like painters, hairdressers or carpenters. Generally speaking, this affects those in the 30-50 age range the most. Tennis elbow usually features pain localized to the lateral region of the elbow at the epicondyle level which may spread down the forearm and is exacerbated by extension and supination movements – including shaking hands or turning a key – as well as feeling of weakness in the arm. Diagnosis is clinical with support from ultrasound scans to assess the integrity of the tendon. Treatment plans focus on a period of rest followed by rehabilitation including: muscle building exercises, stretching, massage, analgesic physical therapies (laser, ultrasound, and shockwave) and also analgesic injections into the tendons. In the (very) rare cases where rehabilitation is unsuccessful, the tendon can be operated on arthroscopically (keyhole surgery).

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.
Frozen Shoulder
Frozen Shoulder
Adhesive Capsulitis of the Shoulder is commonly referred to as ‘Frozen Shoulder’, this condition arises when the glenoid and humeral head adhere to each other, causing a progressive restriction, and low of movement in the shoulder as the joint capsule thickens. Most commonly observed in the 40-60 age range, females, following a period of immobility in the arm, and in those with diabetes, in fact this condition is often the first presentation of late-onset diabetes. This tends to affect the left shoulder more than the right and can often occur without any previous history of trauma or injury.
Capsulitis tends to advance in three stages:
The Cooling Stage
During this stage pain is spread throughout the shoulder, worsening during movement and resulting in a reduced capacity to use the arm. Many patients try to protect their arm and avoid using it which only worsens the condition as it encourages further thickening of the joint capsule.
The Freezing Stage
During this stage pain will slowly build up, and you will notice increased stiffness. Pain can become more localized around the humeral head, worsening throughout the night and therefore impeding sleep. This stage typically lasts between six and nine months.
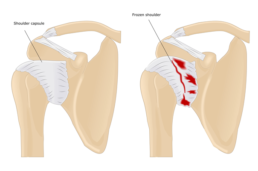
The Thawing Stage
This stage typically occurs naturally, and often times range of motion will gradually improve. However, in some cases it can take up to two years before you regain full movement in the joint.
Diagnosis is usually clinical, but support from ultrasound or MRI scans is sometimes useful. Typically speaking, treatment is conservative, combing anti-inflammatories, physical modalities, joint mobilization and muscular stretching. Surgical treatment is saved for cases where rehabilitation has had little or no effect, here the joint is mobilized through removal of adhesions.

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.
AC Joint Sprain
Acromioclavicular Joint Sprain
The clavicle articulates with the acromian part of the scapula to form the acromio-clavicular joint. This joint is held congruence by the acromio-clavicular ligament and the coracoclavicular ligament, which rises from the coracoid part of the scapula. Injuries to this joint usually arise from a fall onto the shoulder, resulting in the clavicle separating from the acromian. The levels of pain and functional limitation depend on where both ligaments are involved and whether the ligaments themselves are torn, or just stretched. The degree of separation can be measured with a simple X-ray of the shoulder joint, which is often required anyway to check for associated fractures of the clavicle. Ultrasound scans can also be used here. In cases of mild lesions, there is usually only minor swelling of the joint and only partial separation of the two joint surfaces. To measure severity, the injury is graded using the Rockwood scale. This scale ranges from Grade I through Grade VI, increasing in severity with each increment. Typically, most AC injuries are between Grade I and Grade III.

Grade I
The most common type of AC joint injury is a slight displacement of the joint. The AC ligament may be stretched or partially torn. Patients may experience mild tenderness when the joint is touched, and minor pain with arm movement.
Grade II
The joint has become partially dislocated, and the AC ligament is completely torn. Pain in the joint is moderate to severe at this level. A small bump on the top of the shoulder may also be visible as the collarbone is no longer properly secured in place.
Grade III
A complete displacement is evident, as the shoulder falls under the weight of the arm. This forces the clavicle higher, causing a noticeable bump or deformity on the shoulder. Additionally, the AC ligament, coracoclavicular (CC) ligament, and the capsule that surrounds the joint are all torn. Pain is felt upon any arm movement, and is also experienced around the joint and in the area of the CC ligaments.
Injuries with Grades IV to VI are commonly associated with extreme an incident such as a motor vehicle accident.
Treatment of these mild injuries consists of tight strapping of the joint to ensure the ligament fibres remain in place to aid their healing. A period of rehabilitation after this immobilization is important to relieve any stiffness which may have formed in the joint as efficient movement of the shoulder requires a fully functioning acromioclavicular joint. In more complex injuries where the ligaments have completely torn, the clavicle completely separates from the acromian. In these cases, the pain can be particularly intense and surgical intervention is required to restore the continuity of the joint.
Acromioclavicular Joint Sprain
The clavicle articulates with the acromian part of the scapula to form the acromio-clavicular joint. This joint is held congruence by the acromio-clavicular ligament and the coracoclavicular ligament, which rises from the coracoid part of the scapula. Injuries to this joint usually arise from a fall onto the shoulder, resulting in the clavicle separating from the acromian. The levels of pain and functional limitation depend on where both ligaments are involved and whether the ligaments themselves are torn, or just stretched. The degree of separation can be measured with a simple X-ray of the shoulder joint, which is often required anyway to check for associated fractures of the clavicle. Ultrasound scans can also be used here. In cases of mild lesions, there is usually only minor swelling of the joint and only partial separation of the two joint surfaces. To measure severity, the injury is graded using the Rockwood scale. This scale ranges from Grade I through Grade VI, increasing in severity with each increment. Typically, most AC injuries are between Grade I and Grade III.

Grade I:
The most common type of AC joint injury is a slight displacement of the joint. The AC ligament may be stretched or partially torn. Patients may experience mild tenderness when the joint is touched, and minor pain with arm movement.
Grade II:
The joint has become partially dislocated, and the AC ligament is completely torn. Pain in the joint is moderate to severe at this level. A small bump on the top of the shoulder may also be visible as the collarbone is no longer properly secured in place.
Grade III:
A complete displacement is evident, as the shoulder falls under the weight of the arm. This forces the clavicle higher, causing a noticeable bump or deformity on the shoulder. Additionally, the AC ligament, coracoclavicular (CC) ligament, and the capsule that surrounds the joint are all torn. Pain is felt upon any arm movement, and is also experienced around the joint and in the area of the CC ligaments.
Injuries with Grades IV to VI are commonly associated with extreme an incident such as a motor vehicle accident.
Treatment of these mild injuries consists of tight strapping of the joint to ensure the ligament fibres remain in place to aid their healing. A period of rehabilitation after this immobilization is important to relieve any stiffness which may have formed in the joint as efficient movement of the shoulder requires a fully functioning acromioclavicular joint. In more complex injuries where the ligaments have completely torn, the clavicle completely separates from the acromian. In these cases, the pain can be particularly intense and surgical intervention is required to restore the continuity of the joint.

While neck pain is common, it is not normal and should receive professional medical care to determine the cause. Dr. Daniel J. Saenz at MVMT Matters in Sacramento, California, is experienced in accurately diagnosing and treating chronic and debilitating neck pain. Call today to schedule your appointment.